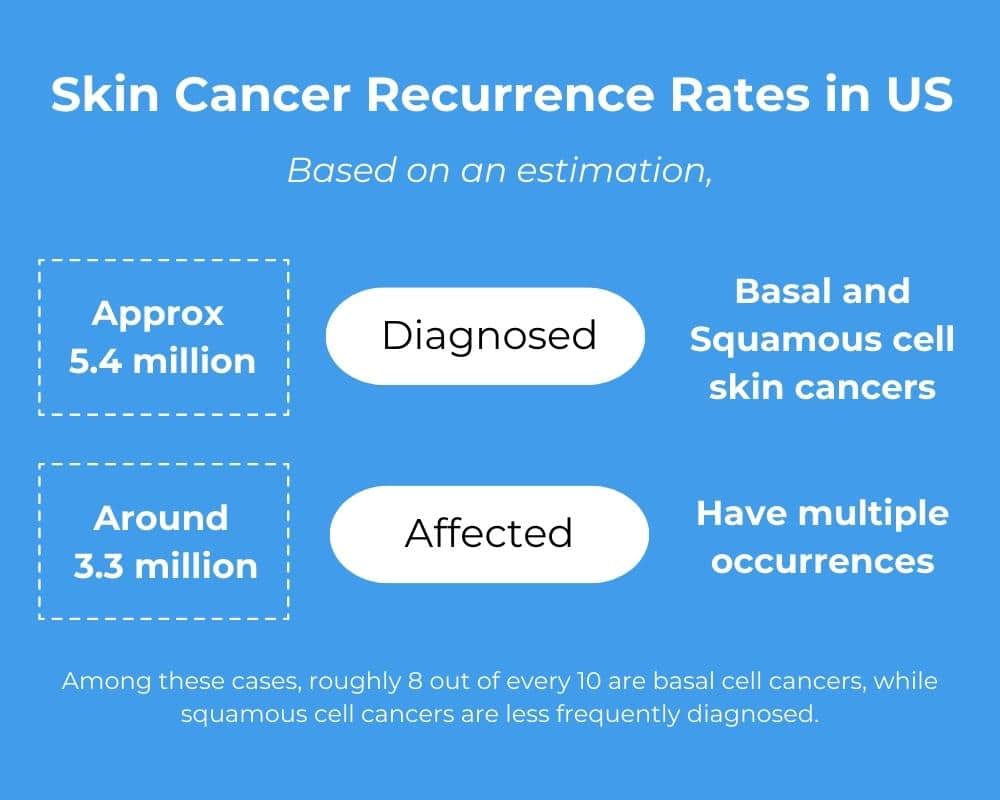
Skin cancer is the most common cancer in the United States with millions of cases diagnosed annually. It’s also one of the most preventable cancers and highly treatable, when found early. While prevention and early detection are essential, understanding the recurrence rate surrounding skin cancer can play a crucial role in our fight against skin cancer. This article will examine skin cancer recurrence statistics and illustrate this often-overlooked facet of the disease.
Be Aware of the Numbers
Did you know that approximately 20% of patients diagnosed with skin cancer will experience a recurrence at some point? Studies suggest that between 30% to 50% of individuals with a non-melanoma skin cancer will experience a second non-melanoma skin cancer within five years. That recurrence risk increases by 2% to 10% for melanoma skin cancer survivors. Regular follow-up appointments, self-examinations of the skin, and sun protection are crucial for the prevention and detection of second skin cancers.
Risk Factors
Exposure to excessive ultraviolet (UV) radiation, such as prolonged sun exposure, sunburns, and tanning beds, is the leading cause of skin cancer recurrence. Recurrent cases can serve as a wake-up call to readers about the importance of sun protection.
Individuals with weakened immune systems, such as organ transplant recipients or those with certain autoimmune diseases, also face a higher risk of recurrent skin cancer. Recognizing and monitoring these vulnerabilities can assist further research into improved preventive measures and tailored treatment options.
Basal Cell Carcinoma Recurrence
Following treatment for basal cell carcinoma (BCC), dermatologists recommend that you undergo a comprehensive skin examination by your dermatologist every 6 to 12 months for the initial five (5) years. It is important to note that recurrence can happen beyond the first five (5) years after treatment and you should consult your doctor for their personalized recommendations on determining the most suitable approach.
BCC recurrence is more common if the tumor is large, has unclear borders, has already recurred once, develops at a site previously treated with radiation therapy, surrounds a nerve, or grows aggressively. Additionally, individuals with a weakened immune system due to medications are more prone to a recurrent BCC.
The chances of BCC recurrence also depends on the patient’s initial treatment received. Mohs surgery has the lowest recurrence rate, with only 1% for primary BCC and 5.6% for recurrent BCC after 5 years. Excision is also highly effective, with a 2% recurrence rate.
Low-risk BCC treatments including curettage and electrodesiccation, topical medication, cryotherapy, or photodynamic therapy are not recommended if the BCC risk of recurrence is high.
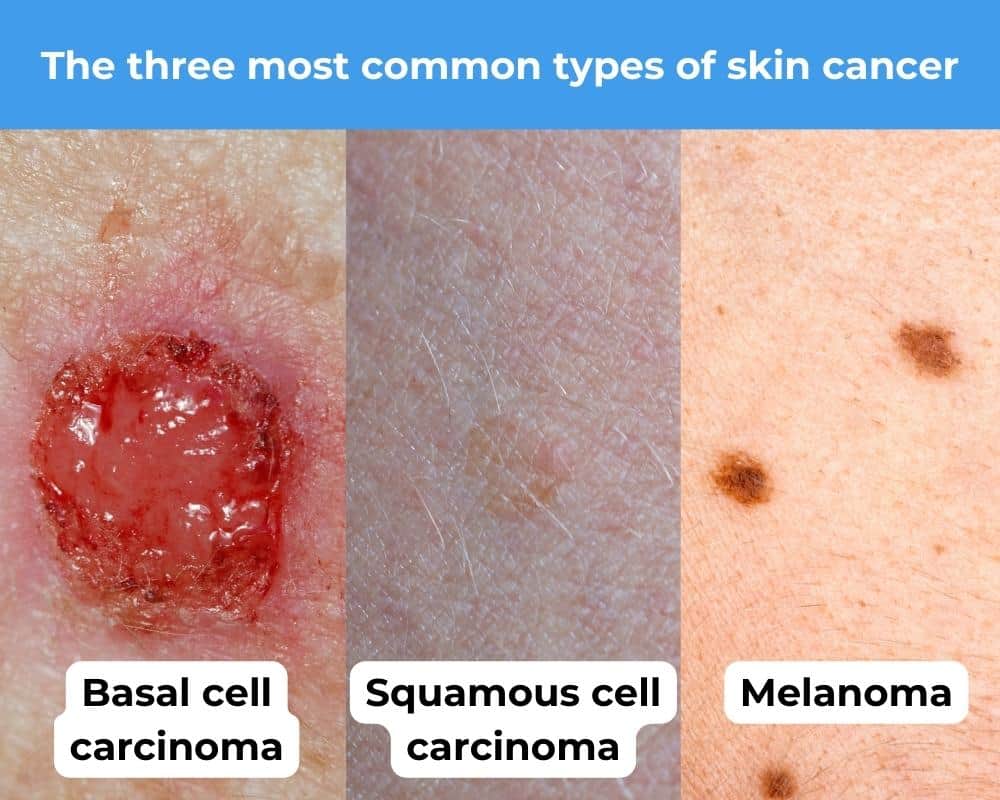
Squamous Cell Carcinoma Recurrence
Following treatment for a local squamous cell carcinoma (SCC), patients are recommended to have a complete skin examination with their dermatologist every 3 to 12 months during the first two years. It is documented that 70% to 80% of SCC recurrences occur within this time frame. Subsequent follow-up visits should be scheduled every 6 to 12 months for an additional three years. If the initial SCC has spread beyond the skin, it may be necessary to have more frequent follow-up visits. Patient’s should consult their doctor to determine their recommendation for your specific situation.
Some SCC tumors are more likely to recur than others. High-risk characteristics of BCC—listed above—are also risky for SCC. Additional risk factors for SCC include:
- Thicker (≥2 millimeters) or more invasive tumor (Clark level IV or V)
- A tumor that has grown around a nerve, lymph vessel, or blood vessel.
- Certain SCC subtypes can be seen under a microscope.
- Poorly differentiated or undifferentiated cells. (Differentiation means how much the cancer cells look like the normal tissue that it came from. Poorly differentiated cells grow and spread more quickly.)
Recurrence rates also vary by the initial treatment. Just like with BCC, Mohs surgery has the lowest 5-year recurrence rate (3%). It is the preferred treatment for SCC that is likely to recur. Excision is also highly effective, with a 5-year recurrence rate of 8%.
Low-risk SCC treatments including curettage and electrodesiccation cryotherapy, photodynamic therapy, and topical medication are not recommended if the SCC risk of recurrence is high.
Melanoma Recurrence
Following the treatment of a melanoma, patients should consult their physician to determine a recommended treatment schedule based on your cancer stage and the development of any symptoms. Here is an explanation of the different cancer stages:
- Stage 0 (melanoma in situ), yearly examinations are advised for life.
- Stage IA-IIA, examinations should be done every 6 to 12 months for five years, followed by yearly examinations for life.
- Stage IIB-IV, examinations are recommended every 3 to 6 months for 2 years, every 3 to 12 months for 3 years, and then yearly examinations for life. Imaging tests may be included in follow-up examinations under certain conditions, such as having symptoms of cancer recurrence or being at high risk of recurrent or metastatic melanoma.
The recurrence of melanoma is significantly influenced by the initial stage of the treated cancer. Melanoma of an early stage has a lower frequency of recurrence with a later time stamp. Conversely, melanoma of a later stage has a higher recurrence rate with a quicker time stamp. It is vitally important for patients to have lifetime follow-up examinations as melanoma can recur even after 10 years from initial treatment.
When it comes to skin cancer, the greater knowledge you have the better. When combining the ever important early detection and prevention of skin cancer with the known risk factors of skin cancer recurrences, we equip ourselves for the successful fight with a relentless opponent, skin cancer.

